A number of our Gynaecologists take a special interest in the diagnosis & treatment of Endometriosis. Read on to learn more about this condition then get in touch to book an appointment with one of our Brisbane Endometriosis specialists.
What is endometriosis?
Endometriosis affects up to one in ten women and is a condition where endometrial like tissue that lines the uterus grows outside of the uterus on the wall of the pelvis, on the ligaments supporting the uterus, on the ovaries and sometimes on the bowel and bladder.
While the exact cause of endometriosis is uncertain, a number of theories exist and it is likely that several factors contribute to the formation of endometriosis. We know that women who have a family history of endometriosis have a 7-8 times higher chance of having endometriosis so genetics play a big role. One theory is that menstruation backwards through the tubes and into the pelvic cavity make endometriosis more likely, however we know that up to 90% of women have some degree of retrograde menstruation so this is not the whole story. Another theory is that cells lining the pelvis undergo changes that convert them into endometrial cells or that endometrial cells are spread via blood or the lymphatic system. There is emerging evidence that endometriosis may be the result of impaired immunity or that environmental exposures when you are still in the womb may make endometriosis more likely. There is still so much we don’t know about endometriosis and there is a pressing need for more research into this mysterious and enigmatic condition.
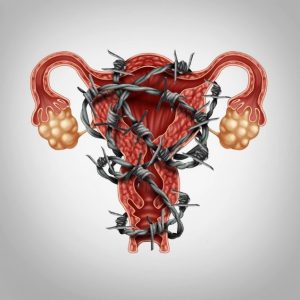
Like the endometrium inside the uterus, the endometriotic implants swell and react to the monthly hormonal cycle. The cells grow and become thicker under the influence of oestrogen and bleed when there is a drop in hormones that corresponds to menstruation. When endometrial cells bleed there is a release of prostaglandin – an inflammatory compound that irritates pain fibers in the area and increases pain. The body responds by surrounding the affected area with scar tissue and inflammation. The formation of scar tissue (adhesions) may result in damage to other pelvic structures and may cause these to stick together. Endometriosis can be deep and infiltrating, or mild and superficial. Interestingly, the degree of severity of endometriosis does not correspond well with the amount of pain women experience. Some women experience debilitating pain and have only a small amount of endometriosis and some may have no symptoms at all and have severe disease. This is a further clue that merely the presence of endometriosis is not the whole story and that the amount or sensitivity of pain nerves could play a role in how different women experience endometriosis.
Endometriosis at its heart seems to be a disease of inflammation and impaired immunity. While the normal hormonal fluctuations in a woman’s cycle can promote the growth of endometrial implants in women who have developed endometriosis, it is the ongoing inflammation that causes the problems not the hormones themselves.
It is prudent to remember that currently there is no cure for endometriosis and both conventional and complementary therapies can only relieve symptoms. By taking a holistic view, we can do a very good job in making sure that you are living a wonderful life with minimal symptoms.
Symptoms:
Symptoms women may experience with endometriosis may include pain with periods, ovulation or sex, pain passing urine or opening bowels or continuous pelvic or lower back pain. Some women may have difficulty falling pregnant. Some women may have pelvic pain at other times in their cycle, nausea and vomiting and even headaches.
It is important to remember that if your periods are extremely painful or you have any of these symptoms which are affecting your quality of life, for example preventing you from attending school or work or doing the things you love, that you seek help from a health professional. If untreated, endometriosis can result in persistent pelvic pain and sometimes in severe cases, infertility.
If you think you may be experiencing some of these symptoms, please ask your GP to consider referring you to an Eve Health gynaecologist for further assessment and investigation.
Further Information on endometriosis can be found at www.pelvicpain.org.au and www.endometriosis.org.au
Diagnosis:
While the gold standard of diagnosis for endometriosis is laparoscopic or keyhole surgery, imaging modalities such as specialised women’s health ultrasound and MRI are becoming more helpful in identifying endometriosis and can pick up around 70% of severe or deep infiltrating endometriosis.
One of the holy grails in endometriosis research is to develop a non-invasive test to diagnose endometriosis so that women don’t need to have invasive surgery just to get a diagnosis. So, watch this space! But for now, while laparoscopy is the only sure way to diagnose endometriosis and can be an important part of your treatment if you do have endometriosis, it is only part of the endometriosis treatment jigsaw puzzle and not the whole solution.
Written By: Dr Tal Jacobson
MA MBBS FRCOG FRANZCOG
Dr Tal Jacobson’s research on endometriosis, pelvic pain, infertility, and laparoscopic surgery has been published in peer reviewed journals and presented at international conferences. Learn more about Dr Tal Jacobson.
More information on the treatment of endometriosis can be found here: Laparoscopic Resection of Endometriosis
Find Us
Comments are closed.
