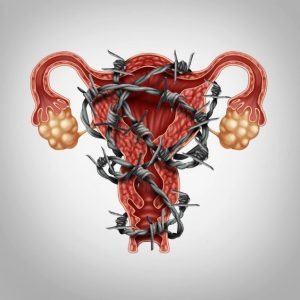
March is Endometriosis Awareness Month, a time to reflect on a disease that affects millions of women globally. Endometriosis (when endometrial like tissue that lines the uterus grows outside of the uterus) was first described over three hundred years ago, but we still know little about how it arises, grows and how it affects individuals.
In part, this is because the term endometriosis has been applied to a group of different conditions with a similar appearance; in part, it is because the clinical picture varies from asymptomatic to disabling, seemingly unrelated to the extent of disease. But mainly, the problem is that the disease is hidden from view and diagnosis is based on a biopsy (a tissue sample) taken at the time of surgery. Moreover, because the disease develops in areas of good blood flow, the diagnosis requires a high degree of skill, as disease frequently needs to be removed from vital structures such as the bowel. This makes the diagnosis challenging. Not surprisingly therefore, the true extent of burden is unknown: up to 1 in 10 individuals assigned as female at the time of birth will have endometriosis. Importantly, endometriosis can occur in transgender, non-binary and gender diverse individuals of any age and has profound effects on partners, families and overall quality of life.
 Symptoms of endometriosis include:
Symptoms of endometriosis include:
- pain (with periods, ovulation, intercourse, when passing urine or opening bowels or continuous pelvic or lower back pain),
- difficulty falling pregnant (infertility), and
- other cyclical symptoms such as bowel or bladder problems.
However, the symptoms of endometriosis are variable and do not always correspond to the severity of disease. It is not unusual to find severe endometriosis in someone who does not have many symptoms. In addition, because pain is a personal experience, it is difficult for people to compare their symptoms. Endometriosis often runs in families, so female relatives, like mothers and sisters, may normalise the symptoms, because they have had the same experience. Not surprisingly, it takes an average of 7 years to make the diagnosis in Australia.
While the exact cause of endometriosis is uncertain, it is likely that several factors contribute to the formation of endometriosis, including genetic or familial predisposition, environmental and immunological factors, reversal of menstrual flow, and changes in the lining of the pelvic cavity.
Endometriosis can be treated by surgery, medical and supportive therapy. Surgical treatment of endometriosis has been shown to reduce pain and improve fertility. In general, surgery is conservative, meaning that the reproductive organs are retained, and is performed by laparoscopy (keyhole surgery). This procedure is performed under a general anaesthetic in an operating theatre. A small incision is made either in or just below the umbilicus. The abdomen is inflated with gas and a camera is inserted to visualise the internal organs. Further small incisions may be made in the abdomen if any abnormalities require treatment. Endometriosis is then cut out (excised) or burnt off (ablated). The wounds are closed in layers. The procedure itself takes thirty minutes or more, but the exact length and need for overnight stay depend on the extent of disease.
The alternative to laparoscopy is open surgery (laparotomy). This is a much more invasive procedure, involving higher complications, increased hospitalisation and recovery. However, in certain situations, a laparotomy may be the most appropriate procedure. More recently, robotic surgery has also been used for endometriosis: this is just a form of endoscopic surgery, where the robot is controlled by the surgeon, who may be in a completely different hospital. The potential of this technology is that it may give rural and remote populations access to advanced endometriosis surgeons, who would normally concentrate in metropolitan centres.
On the other hand, medical treatment has been shown to reduce pain and may have a role in managing disease in conjunction with surgery. Medical treatment has not been shown to improve fertility. Treatments include:
- pain medications,
- hormonal treatments, and
- complementary therapy.
Many women find natural and complementary therapies helpful in the treatment of endometriosis.
Despite effective therapy, there is no cure for endometriosis. Regardless of the type of treatment, it is estimated that 1 in 5 women will have a recurrence of symptoms within five years.
Surgery has been shown to both reduce pain and increase fertility: but the degree of improvement depends on the type of endometriosis, the stage of disease and how it is managed. All gynaecologists are trained in the management of endometriosis, but only a few surgeons treat advanced disease. Advanced endometriosis is usually managed in a multidisciplinary centre, where patients have access to not only gynaecologists, but also an interdisciplinary team of other specialists, nurses, nutritionists, physiotherapists and counsellors.
 Anusch Yazdani is a Founding Director of Eve Health and the Program Director for Endoscopic Surgery and Reproductive Endocrinology for Queensland. He is a subspecialist in Reproductive Endocrinology and Infertility. Anusch is Medical Advisor to Endometriosis Australia and on the Endometriosis Expert Working group for the Department of Health and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG).
Anusch Yazdani is a Founding Director of Eve Health and the Program Director for Endoscopic Surgery and Reproductive Endocrinology for Queensland. He is a subspecialist in Reproductive Endocrinology and Infertility. Anusch is Medical Advisor to Endometriosis Australia and on the Endometriosis Expert Working group for the Department of Health and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG).
For further information, please visit: www.endometriosisaustralia.org
Comments are closed.
